Abstract:
The World Health Organization (WHO) has recently designated the ongoing mpox outbreaks in the Democratic Republic of the Congo (DRC) and other African regions as a Public Health Emergency of International Concern (PHEIC). This designation reflects the escalating severity of the outbreaks, characterized by a surge in cases, fatalities, and the emergence of a new viral strain. While the risk of a global pandemic remains relatively low due to mpox’s transmission dynamics and the availability of countermeasures, the situation necessitates a coordinated international response to contain the spread and mitigate its impact. This article provides an epidemiological overview of the current mpox outbreaks, discusses the factors influencing their pandemic potential, and outlines the public health interventions necessary for effective control.
Introduction
Mpox, a zoonotic viral disease primarily affecting rodents and primates, has emerged as a significant public health concern in recent years. The ongoing outbreaks in the DRC and other African regions, characterized by a significant increase in cases and fatalities, have prompted the WHO to declare a PHEIC on August 16, 2024. This declaration, the highest level of alert issued by the WHO, signifies the gravity of the situation and the urgent need for a coordinated global response to contain the spread of the virus and mitigate its impact.
Epidemiology of Mpox: A Closer Look
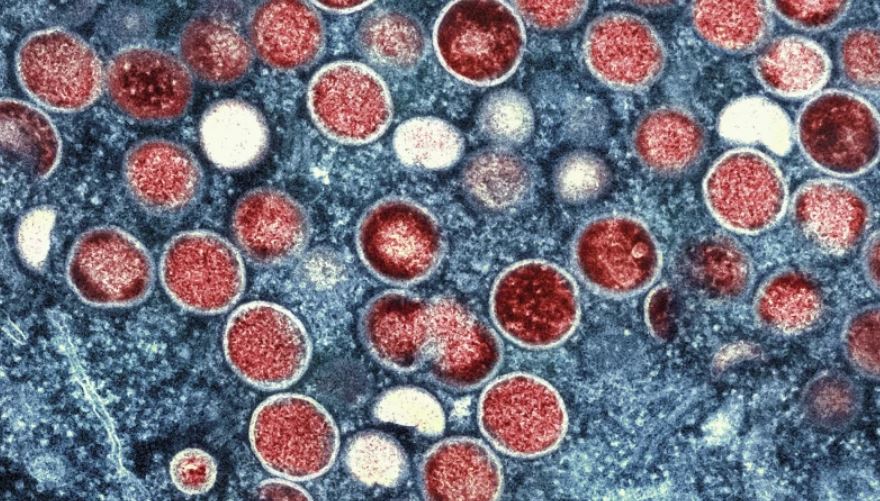
Mpox is primarily a disease of rodents and primates, but it can also infect humans through close contact with infected animals or individuals. The virus is transmitted through direct contact with bodily fluids, lesions, or contaminated materials. Respiratory transmission, although less common, can occur through prolonged face-to-face contact or inhalation of respiratory droplets. The incubation period ranges from 5 to 21 days.
The clinical presentation of mpox is variable, ranging from mild to severe. Initial symptoms include fever, headache, muscle aches, back pain, swollen lymph nodes, chills, and exhaustion. A characteristic rash, often beginning on the face and spreading to other parts of the body, typically follows. The lesions progress through various stages, from macules and papules to vesicles and pustules, eventually forming scabs and healing.
The current outbreaks in Africa are predominantly caused by Clade I of the mpox virus, which is associated with a higher case fatality rate compared to other clades. This, coupled with limited access to healthcare and diagnostic capabilities in some affected regions, contributes to the severity of the outbreaks.
Assessing the Pandemic Potential: A Multifaceted Analysis
While the declaration of a PHEIC for mpox has raised concerns about its pandemic potential, several factors suggest that the risk remains relatively low.
Several factors influence this assessment. Firstly, mpox’s primary mode of transmission, through close physical contact, is less efficient than airborne transmission, which has fueled the rapid spread of recent pandemics like COVID-19. Secondly, the visible skin lesions associated with mpox can act as a deterrent to close contact, potentially limiting its spread. Thirdly, the availability of vaccines and antiviral treatments, although currently limited in some regions, offers a crucial tool for containment and mitigation.
However, the emergence of new mpox variants, as recently reported in Sweden, underscores the need for continued vigilance. The potential for increased transmissibility or virulence in new variants warrants close monitoring and proactive public health measures.
Challenges and Vulnerabilities: Addressing the Gaps
While the overall pandemic risk remains low, the ongoing mpox outbreaks present significant challenges, particularly in resource-limited settings. Limited access to healthcare, diagnostic capabilities, and vaccines poses a major hurdle in effectively controlling the spread of the virus. Additionally, the stigma associated with mpox can hinder efforts to identify and isolate cases, leading to further transmission.
Addressing these challenges requires a multi-faceted approach. Strengthening healthcare infrastructure, improving diagnostic capabilities, and ensuring equitable access to vaccines and treatments are essential steps. Community engagement and education campaigns are also crucial to combat stigma and promote preventive behaviors.
The Global Response: Collaboration and Coordination
The WHO’s declaration of a PHEIC for mpox serves as a call to action for the global community. A coordinated international response is imperative to contain the outbreaks, protect vulnerable populations, and prevent further spread. The WHO is working with national health authorities and international partners to strengthen surveillance, diagnostics, contact tracing, and vaccination efforts.
Research and development of new diagnostics, vaccines, and treatments for mpox are also critical components of the global response. Recent studies have provided valuable insights into the efficacy of existing antiviral treatments. However, further research is needed to develop more effective and accessible interventions.
Public Health Interventions: Empowering Communities
Public health interventions, including health education campaigns and infection prevention and control measures, are essential to mitigating the spread of mpox. Raising awareness about the modes of transmission, symptoms, and preventive measures can empower individuals to make informed decisions and adopt protective behaviors. These interventions can include promoting hand hygiene, encouraging the use of personal protective equipment in healthcare settings, and educating the public about the importance of avoiding close contact with individuals exhibiting symptoms of mpox.
Community engagement is crucial to the success of these interventions. Building trust, addressing concerns, and involving communities in the design and implementation of public health measures can enhance their effectiveness and acceptance.
Conclusion: A Call for Global Solidarity
The current mpox outbreaks in Africa serve as a stark reminder of the interconnectedness of our world and the importance of global health security. While the risk of a global pandemic remains low, vigilance and preparedness are crucial. A coordinated international response, anchored in scientific evidence, equitable access to interventions, and community engagement, is essential to effectively control the spread of mpox and protect the health and well-being of populations worldwide.
Key Learning Points
- The WHO has declared the ongoing mpox outbreaks a PHEIC due to their escalating severity.
- Mpox is a zoonotic viral disease primarily transmitted through close contact with infected animals or individuals.
- The risk of a global mpox pandemic is considered low due to its transmission dynamics and the availability of countermeasures.
- International collaboration and robust public health interventions are essential for effective control.
- Continued research and investment in mpox prevention and control are imperative to address this evolving public health threat.

Basant Kumar Sahoo is a seasoned writer with extensive experience in crafting tech-related articles, insightful editorials, and engaging sports content. With a deep understanding of technology trends, a knack for thought-provoking commentary, and a passion for sports, Basant brings a unique blend of expertise and creativity to his writing. His work is known for its clarity, depth, and ability to connect with readers across diverse topics.