Mpox, a viral zoonotic disease formerly known as monkeypox, continues to cast a long shadow over global public health. The current outbreak in the Democratic Republic of the Congo (DRC) and neighboring regions, fueled by a new, potentially more lethal variant, underscores the urgent need for a comprehensive understanding of this enigmatic pathogen. In this in-depth analysis, we will dissect the complexities of mpox, exploring its mortality rate, available treatments, and the critical public health interventions necessary to curb its spread and mitigate its devastating impact.
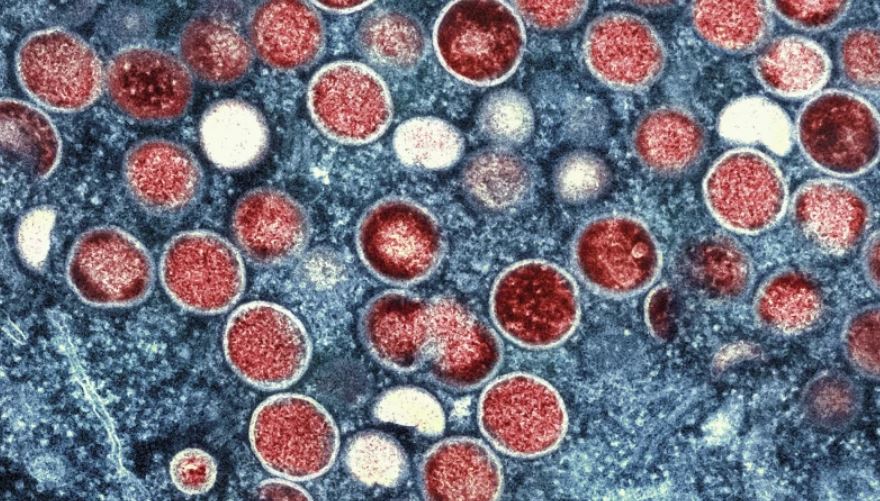
The Enigma of Mpox: Unraveling the Virus
Mpox, a member of the Orthopoxvirus genus, shares a close evolutionary relationship with smallpox. However, unlike its eradicated predecessor, mpox continues to circulate in certain regions, primarily in Central and West Africa. The virus is transmitted to humans through close contact with infected animals or humans, or through contaminated materials.
The clinical presentation of mpox is multifaceted, encompassing a range of symptoms, including fever, headache, muscle aches, back pain, swollen lymph nodes, chills, and exhaustion. A characteristic rash, often beginning on the face and spreading to other parts of the body, typically develops within one to three days of fever onset. These lesions evolve through various stages, from macules and papules to vesicles and pustules, eventually forming scabs that fall off.
The Mortality Rate: A Multifaceted Conundrum
While mpox is generally considered to be less severe than smallpox, it can still lead to significant morbidity and mortality. Studies estimate the fatality rate among individuals infected with the clade I variant, the predominant strain in the current outbreak, to be between 1% and 11%. This wide range reflects several contributing factors that warrant closer examination.
One critical factor is the heterogeneity of affected populations. Infants, children, and individuals with weakened immune systems, such as those living with HIV, are particularly vulnerable to severe and potentially fatal complications. Moreover, pregnant women and individuals with underlying health conditions may also experience more severe disease.
Another contributing factor is the variability in healthcare access and disease surveillance across different regions. In areas with limited healthcare infrastructure and diagnostic capabilities, milder cases of mpox may go undetected, leading to an overestimation of the fatality rate. Additionally, misdiagnosis of mpox symptoms as other diseases, such as measles or chickenpox, can further skew the data.
The Therapeutic Arsenal: A Limited but Expanding Repertoire
In the DRC and neighboring countries at the epicenter of the current outbreak, access to specific mpox treatments remains a significant challenge. Healthcare providers primarily rely on symptomatic management, offering supportive care to alleviate fever, pain, and skin lesions. While crucial for patient comfort, this approach does not directly target the virus itself.
In contrast, countries with more developed healthcare systems have access to antiviral drugs such as tecovirimat. Originally developed for smallpox, tecovirimat has shown promise in animal studies, demonstrating improved survival rates in mpox-infected animals. The drug works by inhibiting a viral protein essential for its spread, thereby curbing viral replication and dissemination.
Other antiviral agents, such as cidofovir, which interferes with viral DNA synthesis, are also being explored as potential treatment options. Additionally, VIGIV, a treatment involving the administration of smallpox antibodies, can be utilized to boost the immune response against the mpox virus.
Evaluating Treatment Efficacy: The Quest for Evidence-Based Medicine
While animal studies suggest the potential efficacy of these treatments, their effectiveness in humans remains under scrutiny. A recent randomized controlled trial in the DRC evaluated the use of tecovirimat in children and adults infected with the clade I variant. The initial results indicated that the drug did not accelerate the healing of skin lesions, a primary clinical manifestation of mpox.
However, the study did observe a lower mortality rate among those receiving tecovirimat, suggesting a potential benefit in reducing severe complications and mortality. Further research is needed to fully elucidate the efficacy and safety of these treatments in diverse patient populations.
The Public Health Imperative: A Call for Coordinated Action
The ongoing mpox outbreak serves as a stark reminder of the persistent threat posed by emerging and re-emerging infectious diseases. It underscores the urgent need for enhanced public health interventions, including:
- Strengthened Surveillance and Diagnostics: Implementing robust surveillance systems to enable early detection, rapid response, and effective contact tracing.
- Improved Access to Treatment: Ensuring equitable access to antiviral drugs and supportive care in affected regions, particularly in resource-limited settings.
- Vaccine Development and Deployment: Accelerating the development and deployment of safe and effective mpox vaccines to protect vulnerable populations and prevent future outbreaks.
- Community Engagement and Education: Raising awareness about mpox transmission, symptoms, and prevention measures to empower individuals and communities to make informed decisions and adopt protective behaviors.
- International Collaboration: Fostering collaboration between global health organizations, governments, and research institutions to facilitate a coordinated and effective response to the mpox outbreak.
A Global Challenge: The Need for Solidarity
The fight against mpox is a global endeavor that transcends national borders. The World Health Organization’s declaration of the current outbreak as a public health emergency of international concern highlights the need for a unified and coordinated response.
Developed nations, with their advanced healthcare systems and research capabilities, have a moral obligation to support affected countries in their efforts to contain the outbreak. This includes providing technical assistance, financial aid, and access to vaccines and treatments. It is only through collective action and global solidarity that we can effectively combat this emerging threat and protect the health and well-being of populations worldwide.
Conclusion: A Beacon of Hope Amidst the Storm
The mpox outbreak presents a formidable challenge, but it is not insurmountable. Through concerted efforts in research, public health interventions, and international collaboration, we can mitigate the impact of this disease and pave the way for a healthier and more resilient future. The road ahead may be long and arduous, but with unwavering commitment and a shared sense of purpose, we can overcome this adversity and emerge stronger than before.
The mpox outbreak is a call to action, a reminder that the fight against infectious diseases is a continuous battle that demands our unwavering attention and dedication. It is a testament to the resilience of the human spirit and our collective ability to confront challenges head-on. As we navigate this complex landscape, let us remember that the pursuit of health and well-being is a universal aspiration, one that transcends borders and unites us all.

Basant Kumar Sahoo is a seasoned writer with extensive experience in crafting tech-related articles, insightful editorials, and engaging sports content. With a deep understanding of technology trends, a knack for thought-provoking commentary, and a passion for sports, Basant brings a unique blend of expertise and creativity to his writing. His work is known for its clarity, depth, and ability to connect with readers across diverse topics.